Table of Contents
The National Practitioner Data Bank (NPDB) is a critical tool in the U.S. healthcare system, designed to enhance patient safety by restricting the ability of healthcare practitioners with negative histories, such as medical malpractice lawsuits or licensure issues, to move unchecked between states. This article provides a comprehensive overview of the NPDB, including its origins, purpose, and the challenges it faces in ensuring the reliability and effectiveness of its data.
Key Takeaways
- The NPDB was established to improve patient safety by preventing practitioners with histories of malpractice or licensure issues from moving between states without disclosure.
- Access to NPDB data is limited to authorized users, and there is a defined process for querying the database to ensure the confidentiality and proper use of the information.
- Despite its goals, the NPDB faces challenges such as reporting compliance, data accuracy, and the timeliness of information, which can affect its effectiveness.
- The NPDB plays a significant role in the credentialing and privileging process, contributing to healthcare quality improvement by aiming to reduce medical errors.
- Future enhancements and policy considerations for the NPDB involve balancing transparency with physician privacy and integrating the database with other healthcare systems for a more comprehensive approach.
Origins and Purpose of the National Practitioner Data Bank

Legislative Background
The National Practitioner Data Bank (NPDB) was established as a direct result of several legislative acts aimed at improving the quality of healthcare and ensuring the competence of healthcare providers. The cornerstone of the NPDB’s legislative foundation is the Health Care Quality Improvement Act (HCQIA) of 1986, which was enacted to restrict the ability of incompetent physicians to move from state to state without disclosure or discovery of their previous damaging or incompetent performance.
Additional legislative measures, such as the Federally Supported Health Centers Assistance Acts (FSHCAA) of 1992 and 1995, extended Federal Tort Claims Act (FTCA) liability protections to eligible health centers, reinforcing the role of the NPDB in maintaining healthcare standards. The 21st Century Cures Act further expanded the scope of the NPDB by including Volunteer Health Professionals (VHPs) under its coverage.
The NPDB serves as a repository of reports containing information on medical malpractice payments and adverse actions related to healthcare practitioners’ licensure, clinical privileges, and professional society memberships, among other data.
The legislative framework of the NPDB reflects a commitment to transparency and accountability in the healthcare system, with the ultimate goal of protecting patients and enhancing the quality of medical care.
Goals for Enhancing Patient Safety
The National Practitioner Data Bank (NPDB) is a vital tool in the pursuit of enhanced patient safety across the healthcare system. Its primary goal is to improve healthcare quality by promoting the competence and integrity of healthcare providers. By maintaining a repository of information on medical malpractice payments, certain adverse actions, and professional society actions related to healthcare practitioners, entities, and suppliers, the NPDB serves as a resource for healthcare organizations to make informed decisions.
The NPDB aims to ensure that healthcare providers who move from state to state or from one healthcare entity to another cannot conceal their previous damaging or incompetent performance records. This transparency is crucial for maintaining trust between patients and healthcare providers and for upholding the standards of care. The following points highlight the key goals of the NPDB in enhancing patient safety:
- Encouraging professional peer review
- Deterring incompetent practice and restricting the ability of incompetent practitioners to move without disclosure
- Improving the quality of healthcare by collecting and disseminating information that promotes competent medical care
The NPDB’s role extends beyond data collection; it is an integral part of the healthcare system’s ongoing effort to maintain accountability and continuous improvement in patient safety.
Scope of Information Collected
The National Practitioner Data Bank (NPDB) is a repository of comprehensive information intended to enhance patient safety and improve the quality of healthcare. The NPDB collects a wide range of data related to healthcare practitioners’ professional conduct and competence. This includes reports on medical malpractice payments, federal and state licensure actions, clinical privileges actions, and professional society membership actions, among others.
The scope of information collected by the NPDB is critical for various stakeholders in the healthcare system. Below is a list of key data categories reported to the NPDB:
- Medical malpractice payments
- Federal and state licensure actions
- Clinical privileges actions
- Professional society membership actions
- Adverse actions related to healthcare education
- Adverse actions related to healthcare fraud and abuse
The data maintained by the NPDB is instrumental in supporting healthcare entities in making informed decisions regarding the credentials of healthcare providers. It serves as a check against practitioners who may pose a risk to patient safety and helps to uphold the integrity of the medical profession.
Accessing and Utilizing NPDB Data
Authorized Users and Entities
The National Practitioner Data Bank (NPDB) is a critical resource for healthcare entities seeking to uphold the standards of patient care through diligent credentialing and privileging processes. Authorized users and entities have the ability to query the NPDB to obtain information that can inform their decision-making regarding healthcare practitioners.
Authorized entities include hospitals, insurance providers, state licensing boards, and other healthcare organizations. These entities must have a legitimate purpose for accessing the data, such as credentialing or investigating professional conduct. It is important to note that authorized agents must query the NPDB separately on behalf of each eligible entity, ensuring that the information is used appropriately and within the confines of the law.
The NPDB serves as a safeguard, providing entities with the information necessary to make informed decisions about healthcare practitioners.
The following list outlines the types of entities that are typically authorized to access NPDB data:
- Hospitals and other healthcare delivery organizations
- Professional societies with formal peer review
- State medical and dental boards
- Health plans
- Federal and state law enforcement agencies
- Federal and state agencies administering government health care programs
Querying the NPDB: A Step-by-Step Guide
After familiarizing oneself with the NPDB Guidebook and understanding the types of information available, querying the NPDB is a critical process for authorized users. The query process is designed to be straightforward and secure, ensuring that sensitive practitioner information is accessed responsibly.
To initiate a query, authorized entities must first register with the NPDB. Upon registration, the following steps are typically involved:
- Log in to the NPDB secure online system.
- Select the appropriate query type based on the information needed.
- Enter the required practitioner or entity details.
- Review and submit the query.
- Await the NPDB’s response, which will be provided electronically.
It is essential for users to ensure that the information entered is accurate and complete to avoid delays or errors in the query response.
Authorized users include hospitals, insurance companies, state licensing boards, and other healthcare entities. They rely on the NPDB to make informed decisions regarding the credentialing, licensing, and employment of healthcare practitioners. The data accessed can have significant implications for patient safety and the quality of care.
Understanding the Limitations of Data Access
While the National Practitioner Data Bank (NPDB) serves as a critical repository for information on medical practitioners, understanding its limitations is essential for effective use. Access to NPDB data is strictly controlled, and only certain entities are authorized to perform queries. These include hospitals, insurance providers, state licensing boards, and certain other healthcare entities.
The NPDB is designed to protect patient safety by providing a centralized source of information on medical malpractice payments and adverse actions related to healthcare practitioners. However, the data is not publicly available, and individuals cannot access their own information without specific procedures.
The NPDB’s confidentiality provisions are intended to balance the privacy rights of practitioners with the need for healthcare entities to make informed decisions.
Authorized users must comply with specific guidelines and legal requirements when querying the NPDB. The following list outlines the key limitations that users may encounter:
- Queries must be made for specific purposes, such as credentialing or licensing.
- Information is not available for general research or public inquiry.
- Users must have a legitimate role in the healthcare industry.
- There are strict penalties for unauthorized use or disclosure of NPDB information.
Challenges and Limitations

Issues with Reporting Compliance
Ensuring consistent reporting compliance within the National Practitioner Data Bank (NPDB) is a significant challenge. The effectiveness of the NPDB is heavily reliant on the accurate and timely submission of reports by healthcare entities. However, discrepancies in understanding the reporting requirements can lead to underreporting or delayed entries, which undermines the database’s role in safeguarding patient safety.
The NPDB’s integrity is compromised when reporting is inconsistent, as it affects the reliability of data used for credentialing and privileging decisions.
To address these issues, resources such as the FTCA Compliance Tool and Educational Training Tracking Tool have been developed. These tools aim to streamline the reporting process and ensure adherence to guidelines:
- FTCA Compliance Tool: Risk Management Annual Report to Board
- FTCA Educational Training Tracking Tool
- FTCA Technical Assistance Resource on Tracking Policies
Despite these measures, the struggle to achieve full compliance persists, highlighting the need for ongoing education and possibly, policy revisions.
Data Accuracy and Timeliness
The integrity of the National Practitioner Data Bank (NPDB) hinges on the accuracy and timeliness of the information it contains. A reliable data management system is crucial for the timely reporting of incidents, which in turn, supports the NPDB’s role in safeguarding patient safety. Efficient data collection and processing are essential components of this system.
To ensure data accuracy, the NPDB must regularly verify the information with the reporting entities. This process can be challenging due to the volume and complexity of data. The following table illustrates the types of data collected and the frequency of verification:
| Data Type | Verification Frequency |
|---|---|
| Medical malpractice payments | Annually |
| State licensure actions | Biannually |
| Federal licensure and certification actions | Quarterly |
| Other adjudicated actions or decisions | As reported |
The NPDB’s effectiveness is directly linked to the quality of its data. Inaccurate or outdated information can lead to misinformed decisions, affecting both healthcare providers and patients.
Challenges in maintaining data accuracy and timeliness can have significant repercussions. For healthcare providers, this may result in unfair characterizations of their professional conduct. For patients, it could mean the difference between choosing a competent provider or one with a questionable history. It is imperative that the NPDB continues to evolve and improve its data management practices to uphold its mission of enhancing patient safety.
Impact on Physician Practice and Mobility
The National Practitioner Data Bank (NPDB) was designed to enhance patient safety by restricting the ability of healthcare practitioners with problematic histories to move unchecked between facilities. However, the impact of the NPDB on physician practice and mobility is complex and multifaceted.
- Physician Relocation: Physicians with reports in the NPDB may find it challenging to relocate or secure new positions, as potential employers have access to their records.
- Career Advancement: Negative entries can stifle career progression, leading to fewer opportunities for professional growth.
- Reporting Variability: Inconsistencies in reporting can result in some physicians being unfairly penalized, while others with similar issues may not be reported at all.
The NPDB’s role in safeguarding patient safety is clear, yet it also raises concerns about fair treatment and the potential for unintended consequences in the professional lives of healthcare providers.
NPDB and Healthcare Quality Improvement

Role in Credentialing and Privileging
The National Practitioner Data Bank (NPDB) plays a critical role in the credentialing and privileging of healthcare providers. Credentialing is the foundational process of verifying a practitioner’s qualifications, including education, licensure, and experience. Privileging follows, granting the practitioner the authority to perform specific procedures or services within a healthcare facility.
- Credentialing involves primary and secondary source verification.
- Privileging requires an assessment of the provider’s ability to perform specific tasks.
Both processes are essential for maintaining high standards of patient care and are mandated for eligibility for Federal Tort Claims Act (FTCA) liability protections. The NPDB serves as a centralized repository of information that aids in these processes by providing data on medical malpractice payments, adverse licensure actions, and other relevant professional conduct or competence issues.
The NPDB’s contribution to credentialing and privileging is a cornerstone of healthcare quality assurance and risk management.
Healthcare facilities must ensure that providers are not only credentialed but also privileged to maintain patient safety and care quality. This requirement is underscored by the need for re-credentialing and re-privileging every two years, emphasizing the ongoing commitment to upholding professional standards.
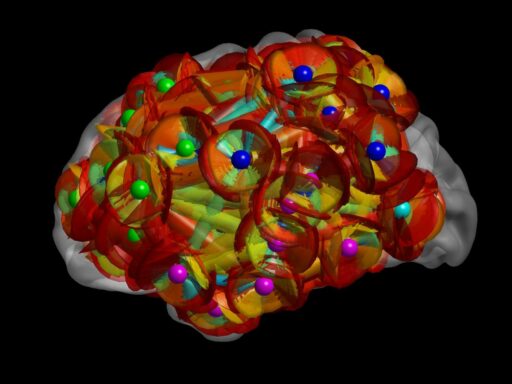
Contribution to Reducing Medical Errors
The National Practitioner Data Bank (NPDB) plays a pivotal role in the healthcare system’s efforts to enhance patient safety by providing a centralized database of information on medical practitioners. The NPDB’s repository of data assists healthcare entities in making informed decisions regarding the credentialing and privileging of medical professionals, thereby contributing to the reduction of medical errors.
By maintaining a record of malpractice payments, adverse licensure actions, and certain disciplinary measures, the NPDB helps to identify patterns that might indicate a higher risk of future errors. This information is crucial for healthcare organizations aiming to uphold high standards of patient care and minimize the occurrence of malpractice.
The NPDB’s impact extends beyond the immediate healthcare setting, influencing broader industry practices. Using evidence-based strategies to help reduce malpractice risk is essential, and the NPDB provides valuable data that supports these efforts.
While the NPDB is a powerful tool, it is not without limitations. It relies on accurate and timely reporting from various entities, and gaps in this reporting can undermine its effectiveness in reducing medical errors.
Defensive Medicine and its Implications
The practice of defensive medicine has significant implications for the healthcare system. Physicians, aiming to avoid malpractice litigation, may order additional tests or procedures that are not necessarily medically indicated. This not only increases the cost of healthcare but may also expose patients to unnecessary risks.
Defensive medicine can lead to a deviation from evidence-based medical practices, as doctors prioritize legal safety over clinical judgement.
While some argue that defensive medicine is a rational response to the litigious environment of healthcare, others see it as a contributor to inefficiencies and inflated costs. The National Practitioner Data Bank plays a role in this dynamic by tracking malpractice payments and adverse actions, which can influence physician behavior.
Certain specialties, such as emergency medicine and obstetrics and gynecology, are more prone to the pressures of defensive medicine due to higher malpractice risk. This can have a profound impact on the quality and delivery of patient care.
Future Directions and Policy Considerations

Proposed Reforms and Enhancements
The National Practitioner Data Bank (NPDB) is poised for significant reforms aimed at improving its utility and reliability. Key enhancements are being considered to address the evolving needs of the healthcare landscape. These include updates to reporting requirements, integration with other databases, and the introduction of new technologies to streamline processes.
- Strengthening the financial alignment initiative
- Expanding the Medicaid Integrity Institute
- Enhancing data resources and technical assistance
The proposed reforms are expected to foster a more transparent and efficient system, ultimately contributing to higher quality patient care.
Further, there is a push for more robust consumer protections and enforcement mechanisms to ensure that the data bank serves its intended purpose without causing undue harm to practitioners. The balance between transparency and privacy remains a critical consideration in the reform process.
Balancing Transparency with Physician Privacy
The National Practitioner Data Bank (NPDB) serves as a repository of information intended to improve healthcare quality and reduce fraud and abuse. However, the balance between transparency and physician privacy is a delicate one. On one hand, the availability of data helps to ensure that healthcare providers with a history of malpractice or misconduct do not simply move from one state to another without scrutiny. On the other hand, the potential for misuse of sensitive information raises concerns about the privacy rights of practitioners.
- Transparency aims to protect patients by providing access to a physician’s history.
- Privacy protects physicians from undue harm due to misinterpretation or misuse of data.
The challenge lies in ensuring that the NPDB effectively deters medical malpractice while safeguarding the reputations of physicians who may have been unfairly reported.
To address these concerns, policies must be carefully crafted to provide necessary oversight without overstepping into areas that could violate privacy rights. The debate continues as stakeholders seek the right equilibrium that upholds the integrity of the medical profession and the safety of patients.
Integrating NPDB with Other Healthcare Databases
The integration of the National Practitioner Data Bank (NPDB) with other healthcare databases could mark a significant step towards a more unified and comprehensive approach to healthcare data management. This integration aims to enhance the quality of care by providing a more complete picture of a practitioner’s history, thereby facilitating better-informed decisions.
- Streamlining data sharing between the NPDB and other databases can reduce administrative burdens.
- It can also improve the accuracy of information, as discrepancies can be more easily identified and corrected.
- A unified system may lead to more effective monitoring of practitioner credentials and histories.
The potential for a centralized healthcare database system to transform patient safety and quality of care is considerable. It could lead to a more proactive approach in preventing medical errors and ensuring that only qualified practitioners are in service.
However, challenges such as data privacy, interoperability standards, and the complexity of merging different data systems must be addressed to realize the full benefits of integration.
Conclusion
The National Practitioner Data Bank (NPDB) serves as a critical repository of information aimed at enhancing patient safety by preventing the mobility of healthcare practitioners with problematic histories. Despite its intent to act as a safety net by tracking medical malpractice lawsuits, licensure issues, and loss of hospital privileges, the system is not foolproof. Challenges in data completeness and accessibility, as well as the potential for defensive medicine, underscore the complexity of ensuring that safeguards are effectively realized. As we have explored, while the NPDB is a valuable tool for credential verification and informed decision-making, stakeholders must remain vigilant and proactive in addressing its limitations to fully protect patients and uphold the integrity of the healthcare system.
Frequently Asked Questions
What is the National Practitioner Data Bank (NPDB)?
The NPDB is a repository established to improve healthcare quality, promote patient safety, and prevent fraud and abuse. It collects information on medical malpractice payments, sanctions taken by boards of medical examiners, and other related actions taken against healthcare practitioners.
Why was the NPDB created?
The NPDB was created to limit the ability of healthcare providers with a history of malpractice or misconduct from moving state to state without disclosure or discovery of their previous damaging performance.
Who has access to the NPDB?
Access to the NPDB is restricted to authorized users such as hospitals, medical boards, and certain other healthcare entities that are involved in credentialing and oversight of healthcare practitioners.
What kind of information can be found in the NPDB?
The NPDB contains reports on medical malpractice payments, federal and state licensure actions, clinical privileges actions, professional society membership actions, and certain other adjudicated actions or decisions.
Can the information in the NPDB affect a physician’s ability to practice?
Yes, the information in the NPDB can impact a physician’s professional career, as it is used by hospitals and licensing boards to make informed decisions regarding credentialing, privileging, and licensure.
Are there limitations to the data provided by the NPDB?
Yes, there are limitations. The NPDB relies on entities to report information accurately and in a timely manner. Incomplete or delayed reporting can affect the comprehensiveness and reliability of the data.